First published on April 9, 2019. This page is updated with new information.
Metabolic Syndrome is a common condition that increases the risk of coronary heart disease, obesity, and Type 2 diabetes.
Metabolic syndrome is present if three of the five conditions are present:
- Fasting blood sugar of more than 100 mg/dl
- Obesity
- High triglycerides
- Low HDL
- Blood pressure of more than 130/85.
A more detailed discussion is available at The Metabolic Syndrome.
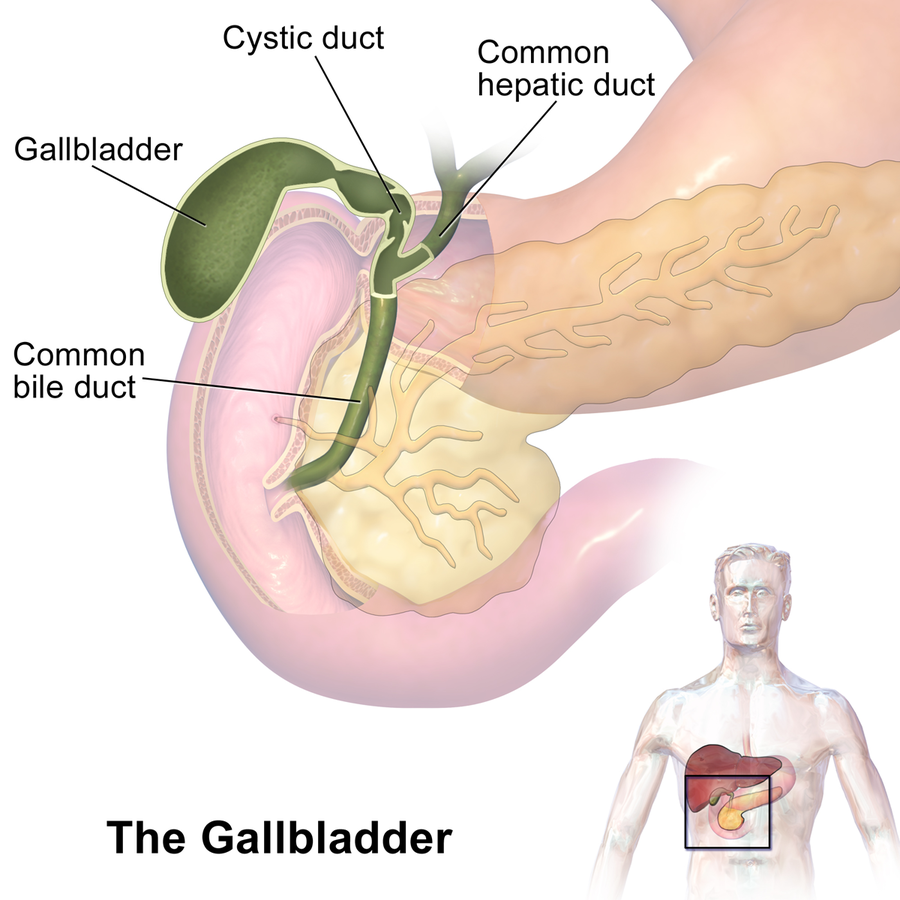
The Gallbladder
The gallbladder is on the right upper part of the abdomen and sits next to the liver. It stores bile produced from the liver that is needed for fat digestion.
If fat is detected in the ingested food, the gallbladder contracts to add bile to the small intestines to help digest fat.
Bile dissolves fat in the diet and acts as an interface between fat and water. It is made of fat, cholesterol, and bile salts.
Gallstones form if there is an imbalance in the composition of bile or if bile accumulates due to a weak gallbladder contraction.
Gallbladder diseases
If bile flow becomes sluggish, then gallstones may form. That condition is called cholelithiasis. By themselves, gallstones do not produce symptoms.
However, if gallstones form in the bile ducts in the liver (choledocholithiasis), they can cause jaundice or yellowing of the skin. It can be life-threatening if it becomes infected (cholangitis).
Gallstones from the bile duct can travel down and block another duct it shares with the pancreas. The pancreas produces enzymes to digest fat, protein, and carbohydrates.
Those enzymes are secreted in the intestines to digest food. If the common duct with the pancreas is blocked, the enzymes will stay in it and inflame it, causing gallstone pancreatitis.
Metabolic Syndrome and Gallbladder diseases
Metabolic syndrome increases the risk of gallstone disease by 3.4 times in men and five times in women thru the following mechanisms.
High triglycerides, elevated blood sugar, and obesity make the gallbladder sluggish and allow bile to accumulate to produce an environment conducive to gallstone formation.
High blood sugar contributes to gallstone formation within the liver by preventing bile acid secretion. Persistent hyperglycemia can lead to insulin resistance and diabetes.
A high carbohydrate diet increases pro-inflammatory cytokines like TNF-α, interleukin -6, and interleukin-1β in the gallbladder tissue.
The results are decreased gallbladder wall movement and less gallbladder absorption of the bile.[7]
High triglycerides increase the fat in the bile to produce cholesterol stones.
The good news is that gallbladder movement improves when high triglycerides are reversed. Either thru medication, fish oil, lower carbohydrate intake, and intermittent fasting.

Gallbladder surgery and Metabolic Syndrome
Most people experiencing problems with gallstones will have a cholecystectomy. A procedure where the gallbladder is surgically removed.
But, that may not solve the metabolic problems. One study showed that people show had cholecystectomy get fatty liver and continue to have metabolic syndrome due to changes in sugar and fat metabolism.
It still looks like prevention is better than surgical treatment as it only provides a partial solution to the problem.
Metabolic Syndrome is associated with other diseases, including cardiovascular disease.
If someone has gallstones, they may have the risk factors to develop coronary artery disease.
Simple blood tests like fasting blood sugar, serum triglyceride, and lipid profile can identify the metabolic syndrome. Check your blood pressure and measure your waistline.
This article is a segment of the series, Diseases Associated with Metabolic Syndrome (MetS).
Don’t Get Sick!
Feel free to share and like. If you find value in this article, you can buy me a coffee!
Related:
- Intermittent fasting results in new and stress-resistant the blood cells
- Intermittent fasting for Post COVID Vaccine Syndrome: Autophagy
- Study: Intermittent fasting results in better COVID-19 outcomes
- Intermittent Fasting while on Diabetes Medications
- Yogurt and Intermittent Fasting Reduced Body Toxins
- Intermittent Fasting Grows New Liver Cells Faster
- Fatty Liver and Metabolic Syndrome
- Fasting and Exercise for Fatty Pancreas
- Triglyceride-Glucose Index tests for insulin resistance and much more
- Metabolic Syndrome and the Pancreas
- Fatty Liver and Metabolic Syndrome
- GERD/Heartburn and Metabolic Syndrome
- Crohn’s Disease and Metabolic Syndrome Part 1
- Crohn’s Disease and Metabolic Syndrome Part 2
- Gallbladder Diseases and Metabolic Syndrome
- Chen CY et al. Age is one of the risk factors in developing gallstone disease in Taiwan. Age Ageing. 1998;27:437–441.
- Chang Y et al. Insulin resistance is associated with gallstones even in non-obese, non-diabetic Korean men. J Korean Med Sci. 2008;23:644–650.
- Kim JM et al. [Association between insulin, insulin resistance, and gallstone disease in Korean general population.] Korean J Gastroenterol. 2007;50:183–187.
- Li-Ying Chen et al. Metabolic syndrome and gallstone disease. World J Gastroenterol. 2012 Aug 21; 18(31): 4215–4220.
- Naim Ata et al. The metabolic syndrome is associated with complicated gallstone disease. Can J Gastroenterol. 2011 May; 25(5): 274–276.
- Nakeeb A, Comuzzie AG, Al-Azzawi H, Sonnenberg GE, Kissebah AH, Pitt HA. Insulin resistance causes human gallbladder dysmotility. J Gastrointest Surg. 2006;10:940–8.
- Pitt HA. Hepato-pancreato-biliary fat: The good, the bad, and the ugly. HPB (Oxford) 2007;9:92–7. [PMC free article] [PubMed] [Google Scholar]
- Smelt AH. Triglycerides and gallstone formation. Clin Chim Acta. 2010;411:1625–1631.
- Di Ciaula A et al. Cholecystectomy and risk of metabolic syndrome. Eur J Intern Med. 2018 Jul;53:3-11. doi: 10.1016/j.ejim.2018.04.019. Epub 2018 Apr 26. PMID: 29706426; PMCID: PMC8118133.
© 2018 – 2022 Asclepiades Medicine, LLC. All Rights Reserved
DrJesseSantiano.com does not provide medical advice, diagnosis, or treatment
As an Amazon Associate, I earn from qualifying purchases.